EMG-driven planning and follow-up of implant-supported maxillary rehabilitation
29 June 2021
Skeletal and postural effects of elastodontic therapy
25 September 2021Case presentation

A case of incongruous prosthetic restoration and dental wear on both arches with altered intermaxillary relationship is presented. Furthermore, an alteration of perio-portesic relationships is shown. The starting state shows a general anamnesis in the normal, with continuous muscle pain apparently due to work stress, such as frequent headaches and muscle pain in the lower third of the face with consequent difficulty chewing. Surface electromyography was used as a tool to monitor muscle function both during initial planning and at delivery of the final prosthetic restoration. Long-term follow-up is then shown in which, thanks to electromyographic control, the functional stability achieved is verified.
Pre-surgical treatment

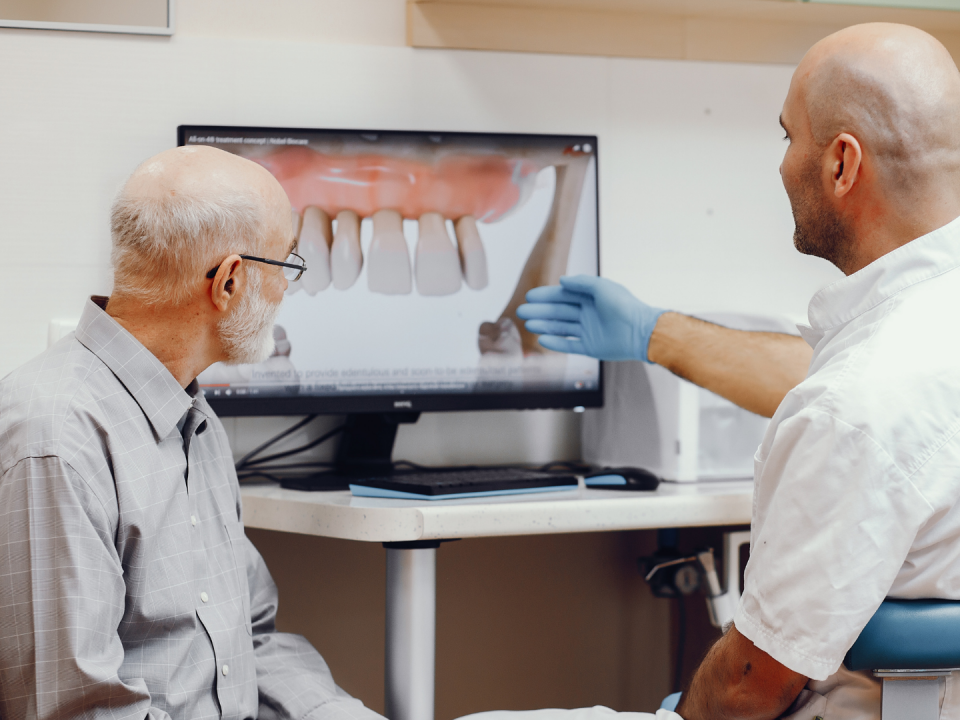
To choose the ideal prosthetic treatment plan for the restoration of the correct spatial relationship of both arches, an aesthetic analysis of the patient was performed with the recording of all photographic records of the current intra-oral situation to identify the prosthetic and aesthetic space to be managed during rehabilitation. Through the objective intra-oral examination, critical aspects were highlighted in terms of periodontal relationships with the prosthetic body and management of intermaxillary relationships. Other critical aspects were the state of abrasion of the masticatory surfaces of the natural teeth and the presence of loss of ceramic structure on the prosthetic devices (attributable to the time of delivery of the prosthetic device). The therapy included the restoration of the correct intermaxillary relationships to the correct vertical dimension tested with Teethan, the restoration of the correct relationships between prosthesis and biological width with resective periodontal surgery and replacement of prosthetic devices. It is also expected the realization of inlays on natural teeth using CAD-CAM methods and new prosthetic crowns in ceramic materials.



Initial diagnostic framing was performed through an evaluation of radiographic status associated with a panoramic and a periodontal survey with bleeding index. To better establish the patient at a functional level, a condylography was performed for an individualized setting of the intermesh cellar relationship in the articulator. This examination allowed to evaluate normal condylar paths and to exclude functional articular pathologies. Subsequently, a cephalometric analysis with VTO was performed to identify how to manage the increased vertical dimension in the lower third of the face.

Thanks to the analysis performed through Teethan, the vertical dimension and the prosthetic space are defined before the intervention, obtaining a general photographic picture of the muscle function in real time.

Temporalis and masseters’ POC indices showed an asymmetry in their function with a very high IMPACT index.



Cephalometric analysis, according to the Vienna School and VTO allowed the calibration of the vertical dimension elevation according to the prosthetic requirements. Digital Smile Design helped to manage aesthetics in the frontal area and to transfer the correct information for the diagnostic creature to the dental technician as well as to communicate the treatment plan to the patient.
Surgery



The periodontal resective surgery, preceded by the replacement of the old prosthetic device with a provisional one, allowed to re-establish the correct peri-prosthetic relationships and to facilitate the surgical maneuvers. The thermostamped template obtained from the diagnostic wax-up guided the surgical phase according to future tooth shapes.

Four weeks after surgery, the temporary was placed with the new intermaxillary relationships in order to ensure a phase of observation and adaptation of the patient. At the same time, work was carried out on the natural teeth with table tops.

The periodontal tissue maturation phase was monitored for 12 months and managed to properly guide soft tissue rebound and interface with prosthetic margins. During this observation period there was also an opportunity to functionalize the temporary to the new vertical dimension obtained.


The realization of table-tops in the diarrheal sectors of the lower arch was carried out with double analog and digital flow to guarantee the best marginal seal and the realization of ceramic devices with controlled thicknesses for the least possible sacrifice of healthy dental tissue.

Monolithic lithium disilicate is treated with adhesive-type cementation, and tabletops were applied in a single session.

After the cementation phase, the temporary was continued in the areas involved in the surgery to avoid altering intermaxillary relationships.

After ten months, the functionalization of the provisional is a parameter that allows for the incorporation of a series of information that is transmitted to the patient, the laboratory, and included in the definitive device.

Subsequently, the Teethan was performed again as a control. The examination showed that the parameters of the temporalis and masseters were within normal range, the center of gravity was slightly posterior, due to the increase in vertical dimension, and the IMPACT was lower than the reference values. The arches were spaced apart while maintaining the absence of torsion.


After ten months of observation, the final stage of the treatment plan is reached. Rotating instruments and ultrasonic inserts under microscopic guidance were used to achieve greater detail and precision. The tissues have responded very well to the entire phase of management of the temporary and preparation of the dental elements following a correct intervention designed ad hoc.
An analogue flow impression of both arches was taken with registration of intermaxillary relationships to transmit all information to the laboratory.

Delivery of lithium disilicate crowns. Layered zirconia only where there are bridges in the posterior sectors.


Cementation is performed by numbering and assigning the crowns, using retractor wires to avoid the infiltration of cement, in some cases transparent and difficult to detect radiographically in periodontal tissue.
Definitive prosthesis

Seamless integration of the devices in the upper and lower arch was assessed with radiographic and photographic aids.

View of the upper and lower arch with active and passive centric arches conforming to the final result of the definitive prosthesis and subsequent aesthetic integration of the work performed in the lower third of the patient’s face.

At the final delivery of the prosthetic device, Teethan examination was repeated and showed a general
picture of all the initial values within the norm, the work of the muscles is symmetrical and there is no torsion.

The pie chart shows that everything is proceeding correctly, and the last photographs show the change that there has been between the initial intra-oral situation and that at the delivery the prosthetic devices.